By Nicholas Metzger, RN, MBA, CEN; Michelle Gunnett, RN, MSN, CEN; Desiree Hadden, RN, BSN; Bruce Friedberg, MD, FAAEM; and Jaime Rivas, MD, FACEP
Lack of inpatient capacity is a major contributor to emergency department (ED) crowding. The usual solution is to work toward shorter inpatient length of stay (LOS) and more efficient discharges. But the ED team at Palomar Health in San Diego County is finding success with the opposite approach. Specifically, they're applying an evidence-based protocol to safely minimize preventable admissions while ensuring patients still get the care they need.
The following is based on a poster presented at Vituity's annual conference.
Background
Palomar Health is the largest hospital district in California, serving communities in an 850-square-mile area. Its trauma center covers more than 2,200 square miles of South Riverside and North San Diego Counties. The district includes two hospitals: 288-bed Palomar Medical Center (PMC) in Escondido and 107-bed Palomar Medical Center Poway.
For the past several years, Palomar Health has been focused on improving ED turnaround times. To this end, we've created a standardized discharge process, placed a provider in triage during peak hours and much more.
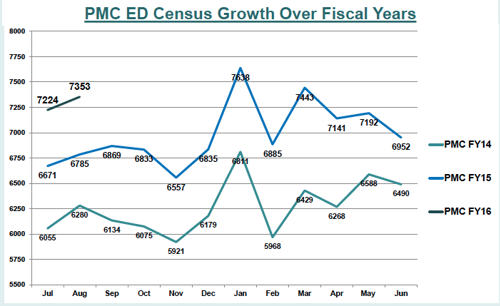
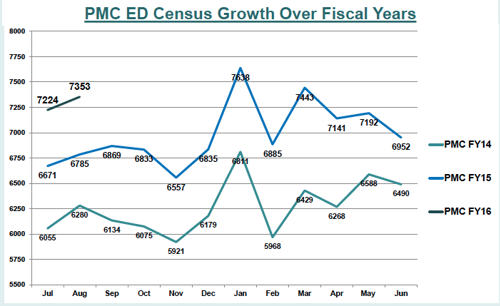
A key part of this work has focused on prevention of unnecessary hospital admissions. This is a particularly salient issue for Palomar Health, because in recent years, inpatient beds across the system have generally been filled while ED census has risen.
By preventing unnecessary admissions, our team hoped to reduce boarding of patients in the ED, a practice which exacerbates ED crowding and can lead to poorer outcomes.
To prevent unnecessary admissions, we focused on coordination across the care continuum — an approach endorsed by the American Nurses Association, Emergency Nurses Association and other professional societies.
Why Chest Pain?
Each year, 8 to 10 million Americans present to the ED with chest pain, representing about 5.5 percent of visits. Occasionally, this pain signals a true emergency. However, a robust body of evidence demonstrates that many of these patients are at low risk for adverse events and can be safely treated in the outpatient setting.
Some facts about chest pain and its management:
- 50 percent of all chest pain patients who present to the ED receive lengthy inpatient cardiac evaluations.
- Less than 10 percent of those patients have acute coronary syndrome (ACS) requiring any further intervention.
- Annual cost of chest pain patients in EDs is estimated at $10–13 billion.
- Hospital admissions criteria for chest pain are often weighted toward “dynamic ECG changes" and/or "positive biomarkers.” However, negative results do not completely rule out ACS.
- Missed ACS is the No. 1 cause of ED malpractice claims.
- For these reasons, follow-up care is essential for chest pain patients discharged from the ED.
Description of Project
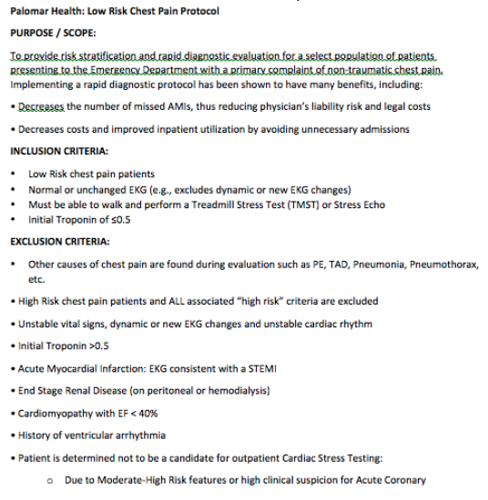
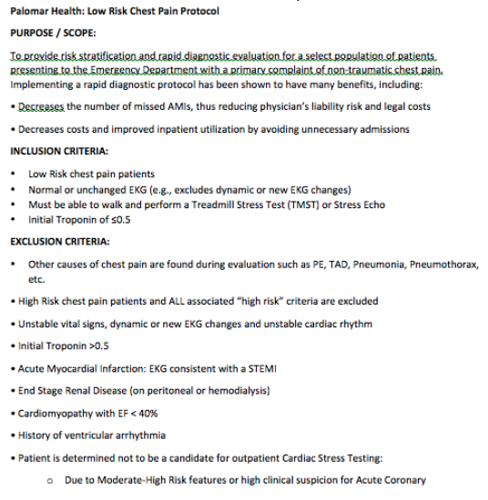
To improve the management of chest pain patients, we developed a new Low-Risk Chest Pain Protocol treatment model. Such protocols are well supported by research and have been successfully implemented by other EDs (though to our knowledge, none in Southern California).
ED physicians championed the idea and conducted much of the early research and development for the project. Later, the system's chief administrative officer helped us gain buy-in from the cardiology department, Kaiser Permanente and Graybill medical groups (whose patients we often serve), direct patient care staff and other stakeholders.
A brief overview of the protocol:
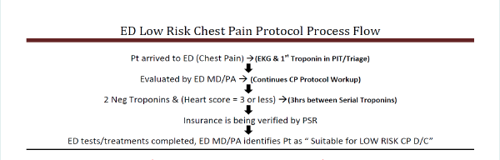
An overview of the process flow:
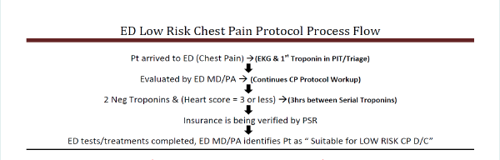
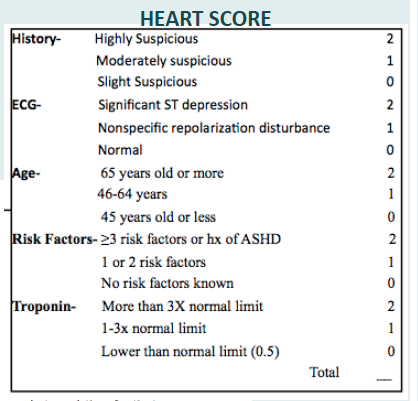
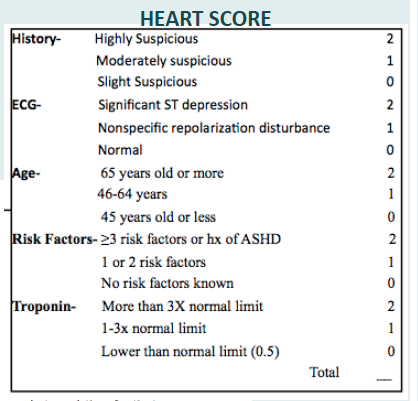
The Heart Score referenced in the protocol is an assessment specifically designed to stratify all ED patients with chest pain. Multiple multicenter international studies have found Heart Score to be a strong predictor of event-free survival on one hand and potentially life-threatening cardiac events on the other.
The protocol also specifies a process for arranging follow-up care. Our ED staff works directly with Kaiser Permanente and Graybill to facilitate scheduling of a post-discharge stress test within 72 hours. All other patients are scheduled with Palomar Health cardiologists for testing.
Staff Roles
ED provider
- Evaluates patient for potential Low-Risk Chest Pain Protocol and ED discharge.
- Reviews Low-Risk Chest Pain pathway with patients, writes appropriate discharge orders.
- Verifies primary care provider/insurance group with patient at discharge.
- Ensures patient information sheet is provided to appropriate cardiology office.
ED Scribe
- Reviews patient's insurance to verify correct discharge instructions are written.
Nursing unit secretary/patient service representative
- Ensures patient’s insurance is verified and accurate upon arrival to the ED.
- Assists in faxing, emailing and follow-up with cardiology offices to provide patient information for those needing outpatient stress test follow up.
ED patient care RN
- Reviews chart to ensure discharge instructions are transmitted to patient's primary care provider.
- Reviews follow-up instructions with patients at discharge, reminding them that they will have an outpatient stress test within 72 hours.
ED clinical supervisor
- Conducts patient callbacks to gauge compliance with follow-up recommendation.
Outcomes and Results
In its first two months, the protocol allowed us to more effectively address ED issues of input, throughput and discharge, thus providing a more optimal patient experience.
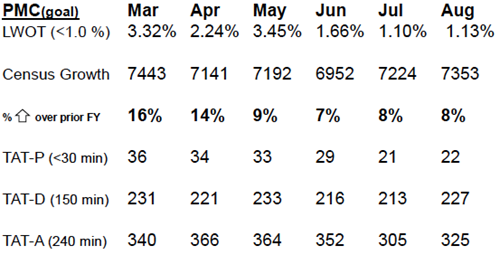
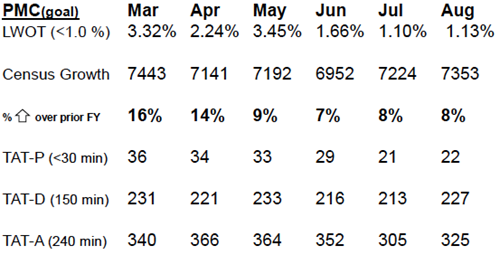
Our initial turnaround time to discharge (TAT-D) results were better than expected upon review of the initial data set, especially in light of our trend toward increasing census. However, we do expect to see a slight increase in TAT-D specifically for this chest pain patient population, given the time it takes to complete the protocol testing.
This protocol has had the unintended benefit of increasing nurse-physician collaboration. The process brings both disciplines together at the bedside to determine the plan of care. It also creates opportunities to practice Team Discharge. As a result, providers and nurses better understand one another's roles and have a deeper appreciation for the ways in which healthcare delivery is changing. This growing spirit of openness and collaboration has spilled over into other ED quality initiatives in positive ways.
Protocol implementation continues to be a work in progress. The ED leadership team audits feedback from community providers. We also meet regularly with cardiology and the administration in order to refine our process and ensure that our patients are receiving appropriate follow-up care.
Updates
Since our poster presentation, the PMC ED has continued the Low-Risk Chest Pain Protocol with great success. The program is currently being implemented at our second ED at Poway.
Due to the number of ED throughput initiatives currently underway, it's difficult to measure the protocol's direct impact on turnaround times. However, there has been an overall trend toward improvement despite rising volumes. Feedback from patients has generally been positive, and the program's safety record has been strong.
Some lessons learned:
- Take the time to gain buy-in. In our case, it took about 1.5 years of meetings and discussions to get all stakeholders on board.
- Plan ahead for resource allocation. As we've expanded the protocol to Pomerado, we've had to adjust staffing to ensure we have the resources to offer stress tests at that location.
- Discharging chest pain patients may cause anxiety for providers, nurses and staff. Before implementing the protocol, provide education to help them understand the rationale and research basis.
- Patients are generally happy to be discharged, as long as they understand that they are at low risk for a cardiac event. Scripting can help providers and nurses communicate the key points in a way that patients understand.
Originally posted Jan. 14, 2016. Updated April 30, 2018.