Vituity’s Director Seth Thomas, MD, and Paul Rains, President, St. Joseph’s Behavioral Health Center presented at the 2020 National Alliance on Mental Illness (NAMI) Conference. Dr. Thomas completed a six-month acute behaviorial health pilot at nine Dignity Health emergency departments. Through the use of Vituity’s Emergency Psychiatric Intervention (EPI) approach, locations improved the patient and staff experience and increased cross-team collaboration to identify and provide for patient needs. Learn about the results in Psychiatric Emergency: Changing the Culture in Our EDs.
Skyrocketing demand for acute behavioral health care falls heaviest on our nation’s emergency departments (EDs). Recent studies show that the average behavioral health patient spends an average of 11.5 hours in the ED. The practice of holding patients while waiting for consults and admissions creates congestion, drives up costs, and delays care for all patients.
How can hospitals and health systems respond? To get some answers, we sat down with Seth Thomas, MD, FACEP, Vituity’s Director of Quality and Performance. In this conversation, he explains how an integrated approach to treating psychiatric emergencies can often help patients avoid unnecessary admissions by providing the right care at the right time.
In your opinion, what are the biggest challenges in behavioral health care delivery today?
Seth Thomas: One of our biggest challenges is providing differentiated care. Think of it this way. When a patient comes to the ED with chest pain, we risk-assess them based on their history, physical, and selected testing and treat them accordingly. Not every chest pain patient needs a cardiology consult or an angiogram or an inpatient admission. Some can be treated and discharged for outpatient follow-up.
Contrast that with our approach to behavioral health patients. EDs tend to put every mental health and substance abuse patient into the same bucket. The majority of behavioral health patients wait for psychiatry consults or crisis worker evaluations—even if they’re coming in just to refill a prescription.
During this long wait, they’re rarely treated or re-evaluated. If they become agitated and their behavior escalates, which is common, they’re sedated, automatically lengthening their stay by 6 to 8 hours. As a result of not receiving the appropriate and timely care, a disproportionate number of these patients end up being admitted.
This undifferentiated approach is a grave disservice to both patients and providers. It has the potential to delay care for all patients. It also puts a tremendous burden on the hospital. One study found that each behavioral health visit to the ED prevents 2.2 bed turnovers and results in a loss of $2,264.
Why do so many EDs struggle to differentiate behavioral health care?
Seth Thomas: Often, it comes back to the stigma around mental health. Sadly, there are people out there who believe that mental health and substance abuse patients don’t belong in EDs. In their eyes, these patients are just passing through on their way for treatment somewhere else. When ED teams don’t take responsibility for assessing and treating behavioral health patients or easing their suffering, the patients, the teams, and the hospitals suffer.
Yet when EDs do want to help, they feel unprepared and under resourced. As an emergency medicine resident, I got very little training on how to treat patients with a behavioral health crisis. I was never taught how to assess them or manage their symptoms, like agitation. Nor was I taught how to start psychiatric medications in the ED, which can make a big difference in the patient’s outcome.
And finally, there’s a lack of standardized tools to help us assess and treat behavioral health patients appropriately. With a chest pain patient, I can use an evidence-based algorithm to assess risk and guide my decision-making. But when a patient is depressed or showing signs of psychosis, there’s not much to go on.
The result is that every provider handles these cases differently. Sometimes an individualized approach is appropriate in the ED. But when there are no standards at all, it leads to huge gaps in care.
What kind of approach to behavioral health care will most benefit providers and patients?
Seth Thomas: There’s understandably been a huge push to integrate psychiatry into ED care. Solutions like telepsychiatry, consult liaison services, and crisis stabilization units all benefit patients with complex health needs. However, we also need solutions to help us manage less acute patients who may not require all these overtaxed resources.
One solution that addresses these problems is Vituity’s Emergency Psychiatry Intervention (EPI) program. EPI empowers ED care teams through clinical education, best-practice implementation, and leadership training. It provides teams with pathways to assess risk and provide early intervention. This includes identifying and stabilizing low- to moderate-risk patients, who in many cases can be safely discharged from the ED.
The EPI model has many benefits. Behavioral health patients receive early and appropriate treatment that eases their suffering. Providers and staff feel more satisfied in their roles knowing they have the tools to help. The process reduces wait times and delays for all patients, improving outcomes and satisfaction. And finally, the process saves hospitals money and resources by improving throughput and freeing psychiatric consultants to focus where they are truly needed.
What results have you seen from the use of EPI at practice locations?
Seth Thomas: Starting in late 2018, four EDs in the Chicago-based AMITA Health system participated in the launch of EPI. All of these departments were seeing high volumes of behavioral health patients. They were looking for risk stratification methods and new medication protocols that would lead to more accurate diagnoses, better treatments, and faster discharge rates.
In particular, the ED team at AMITA Health Saint Joseph Hospital was facing a number of challenges, including turnover in the hospital’s inpatient behavioral health unit. They needed resource-neutral solutions that could be fully implemented within the ED. To this end, they decided to focus on developing a risk-stratification process and creating discharge resources.
The team also decided to promote use of second-generation antipsychotic medications to treat agitation and anxiety. These drugs are less sedating than older antipsychotics, so they don’t increase patients’ lengths of stay unnecessarily. They also began offering them the medications earlier and in oral formulations, thereby further reducing oversedation and coercion.
After undergoing EPI training and implementing Vituity’s toolkit, AMITA Saint Joseph reduced ED length of stay for low-risk patients by 38% and medium-risk patients by 20%. What’s more, none of the discharged patients “bounced back” unexpectedly.
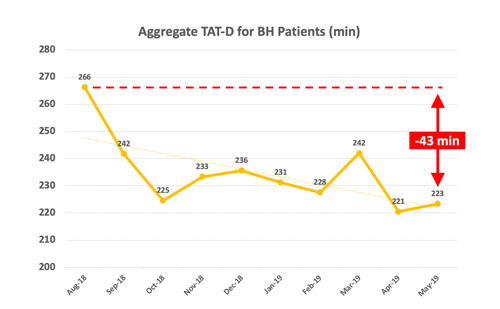
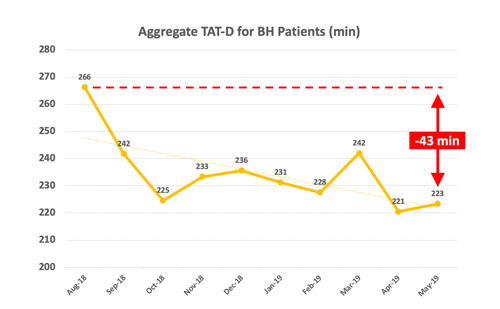
The other three hospitals in the pilot saw similar results. The ED at AMITA Health Saint Francis Hospital cut their length of stay for discharged behavioral health patients in half, reducing it from 300 minutes to 150. Together, the four participating hospitals reduced their average wait times for this population by an impressive 43 minutes.
In the following graph, “TAT-D” stands for turnaround time to discharge.
Caring for behavioral health patients is a national problem. Why did Vituity take on this challenge?
Seth Thomas: I think the number one quality that sets Vituity apart is that we’re a physician-led and -owned organization. This means that our physicians have a very personal stake in our practices and in our communities. We are motivated to innovate, experiment, and come up with creative solutions to the most challenging problems we see every day.
For example, back in the early 2000s, our front-line providers created the Rapid Medical Evaluation (RME)® process. This involves assessing patients quickly and stratifying them into care pathways based on acuity. Contrary to historical practice, low-acuity patients need not be bedded. Instead, they are kept “vertical” between assessments, treatments, and procedures. The practice has been successfully tested for every ED size and patient population. It eventually spread beyond Vituity, and today hospitals use it across the country.
EPI was born when Vituity providers in the emergency room began applying RME principles to the care of psychiatric patients. The process is entirely designed by front-line ED providers and nurses who work with this patient population every day. Vituity’s transformation team and practice management specialists helped to refine and validate EPI and shaped it into a scalable program that can be easily replicated at new locations nationwide.
Another quality that sets Vituity apart is our patient-centered culture. Because we are wholly physician-owned, there are no investors, stakeholders, or non-physician executives looking over our shoulders and pressuring us about profits. We are free to focus 100% of our energy and passion on delivering great patient care. It’s an ideal way to practice medicine, and we see the results every day in our satisfied hospital partners and patients.
Implementing EPI requires formalized training for emergency providers as well as access to dedicated behavioral health services. To learn more, watch the webinar hosted by Becker’s Hospital Review, or contact solutions@vituity.com.
This content was originally posted on November 1, 2019.